| BASELINE CHARACTERISTICS | OPDIVO (n=532) | PLACEBO (n=262) |
|---|---|---|
| Median age (range), years | 62 (26–82) | 61 (26–86) |
| Male, % | 84 | 85 |
| Race,* % White Asian |
81 16 |
82 13 |
| ECOG PS, % 0 1 |
58 42 |
60 40 |
| Disease stage at initial diagnosis, % II III |
34 66 |
38 62 |
| Tumor location, % Esophagus Gastroesophageal junction |
60 40 |
59 41 |
| Histology, % Squamous cell carcinoma Adenocarcinoma |
29 71 |
29 71 |
| Pathologic lymph node status ≥ypN1, % | 57 | 58 |
| Tumor cell PD-L1 expression,† % ≥1 % <1 % Indeterminate/nonevaluable |
|
|
OPDIVO Qvantig™ (nivolumab + hyaluronidase-nvhy) is approved as a subcutaneous injection
Adjuvant Treatment of Completely Resected ESO or GEJ Cancer
The first and only adjuvant immunotherapy to double median disease-free survival vs placebo1,2*

*Primary analysis.2
INDICATION OPDIVO® (nivolumab) is indicated for the adjuvant treatment of completely resected esophageal or gastroesophageal junction cancer with residual pathologic disease in adult patients who have received neoadjuvant chemoradiotherapy (CRT).
CHECKMATE 577: IN THE ADJUVANT TREATMENT OF ADULT PATIENTS WITH COMPLETELY RESECTED EC OR GEJC WITH RESIDUAL PATHOLOGIC DISEASE FOLLOWING NEOADJUVANT CRT
A phase 3 study evaluating OPDIVO following neoadjuvant CRT + surgery to reduce the risk of recurrence or death in EC/GEJC1-3
PATIENTS INCLUDED IN THE TRIAL HAD RESIDUAL PATHOLOGIC DISEASE1-3

- This trial excluded patients who did not receive concurrent chemoradiotherapy prior to surgery, had stage IV resectable disease, autoimmune disease, or any condition requiring systemic treatment with either corticosteroids (>10 mg daily prednisone or equivalent) or other immunosuppressive medications1
- Disease-free survival is the time between date of randomization and date of first recurrence or death1
- Median follow-up was 32.2 months3
1L=first-line; CRT=chemoradiotherapy; EC=esophageal cancer; ECOG PS=Eastern Cooperative Oncology Group Performance Status; GEJC=gastroesophageal junction cancer; IV=intravenous; PD-L1=programmed death-ligand 1; q2w=every 2 weeks; q4w=every 4 weeks.
Patient baseline characteristics in Checkmate 5772
*Other races not shown.2
†Tumor cell PD-L1 expression determined from surgical specimen by the PD-L1 IHC 28-8 pharmDx assay (Dako).2
IHC=immunohistochemistry.
OPDIVO doubled median disease-free survival vs placebo1-3
MEDIAN DISEASE-FREE SURVIVAL* IN ALL RANDOMIZED PATIENTS

31% reduction in the risk of recurrence or death with OPDIVO vs placebo1
*Per investigator assessment.1
†The boundary for statistical significance at the pre-specified interim analysis required the P value to be less than 0.036.2
‡Median follow-up of 32.2 months.3
Primary analysis: DFS benefit was observed regardless of tumor PD-L1 expression2:
- PD-L1 ≥1% (n=129) mDFS: 19.7 mos (95% CI: 11.3–NA) with OPDIVO vs 14.1 mos (95% CI: 5.5–22.8) with placebo; unstratified HR=0.75 (95% CI: 0.45–1.24)2,4
- PD-L1 <1% (n=570) mDFS: 21.3 mos (95% CI: 16.3–34.0) with OPDIVO vs 11.1 mos (95% CI: 8.3–15.2) with placebo; unstratified HR=0.73 (95% CI: 0.57–0.92)2,4
- PD-L1 indeterminate/nonevaluable (n=95) mDFS: NR (95% CI: 13.3–NA) with OPDIVO vs 9.5 mos (95% CI: 3.4–NA) with placebo; unstratified HR=0.54 (95% CI: 0.27–1.05)2,4
- Based on an exploratory, pre-specified analysis2
mDFS by time from complete resection to randomization2:
- <10 weeks (n=256): 24.0 mos (95% CI: 13.7–NA) with OPDIVO vs 14.1 mos (95% CI: 8.31–26.25) with placebo; unstratified HR=0.84 (95% CI: 0.57–1.22)2,5
- ≥10 weeks (n=538): 21.4 mos (95% CI: 16.6–NA) with OPDIVO vs 10.8 mos (95% CI: 7.59–13.93) with placebo; unstratified HR=0.66 (95% CI: 0.52–0.84)2,5
- Based on an exploratory analysis2
- In Checkmate 577, enrollment required complete resection within 4 to 16 weeks prior to randomization1
14-month follow-up analysis: increased DFS regardless of PD-L1 expression3,5:
- PD-L1 ≥1% (n=129) mDFS: 28.3 mos (95% CI: 13.3–NA) with OPDIVO vs 10.2 mos (95% CI: 5.5–22.8) with placebo: unstratified HR=0.68 (95% CI: 0.42–1.10)
- PD-L1 <1% (n=567) mDFS: 20.8 mos (95% CI: 16.0–33.7) with OPDIVO vs 11.0 mos (95% CI: 8.0–15.1) with placebo; unstratified HR=0.70 (95% CI: 0.56–0.87)
- PD-L1 indeterminate/nonevaluable (n=98) mDFS: 26.6 mos (95% CI: 14.1–NA) with OPDIVO vs 9.9 mos (95% CI: 3.4–NA) with placebo; unstratified HR=0.64 (95% CI: 0.34–1.20)3,5
mDFS by time from complete resection to randomization3,5:
- <10 weeks (n=256); 24.0 mos (95% CI: 14.8–NA) with OPDIVO vs 12.7 mos (95% CI: 8.3–NA) with placebo; unstratified HR=0.85 (95% CI: 0.59–1.23)3,5
- ≥10 weeks (n=538): 21.3 mos (95% CI: 16.6–34.0) with OPDIVO vs 9.3 mos (95% CI: 7.6–12.6) with placebo; unstratified HR=0.63 (95% CI: 0.50–0.79)3,5
- Based on a 32.2 month median follow-up analysis3
- In Checkmate 577 enrollment required complete resection within 4 to 16 weeks prior to randomization1
CI=confidence interval; DFS=disease-free survival; HR=hazard ratio; mDFS=median disease-free survival; mo=month; NA=not available; NR=not reached.
Select Important Safety Information
Serious Adverse Reactions
In Checkmate 577, serious adverse reactions occurred in 33% of patients receiving OPDIVO (n=532). A serious adverse reaction reported in ≥2% of patients who received OPDIVO was pneumonitis. A fatal reaction of myocardial infarction occurred in one patient who received OPDIVO.
Common Adverse Reactions
In Checkmate 577, the most common adverse reactions (≥20%) in patients receiving OPDIVO (n=532) were fatigue (34%), diarrhea (29%), nausea (23%), rash (21%), musculoskeletal pain (21%), and cough (20%).
Please see additional Important Safety Information below.
Flexible dosing schedule and faster* delivery to meet the needs of your patients6
OPDIVO is still available as an IV infusion. View OPDIVO IV dosing schedule >
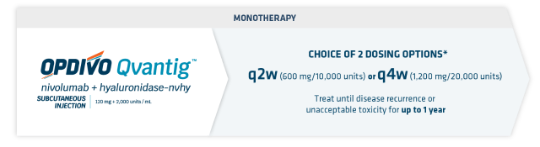
INDICATION OPDIVO Qvantig (nivolumab + hyaluronidase-nvhy), as monotherapy, is indicated for the adjuvant treatment of completely resected esophageal or gastroesophageal junction cancer with residual pathologic disease in adult patients who have received neoadjuvant chemoradiotherapy (CRT).
- OPDIVO Qvantig is administered as a 3- to 5-minute subcutaneous injection6
- Review the Full US Prescribing Information for recommended dosage information for OPDIVO Qvantig
- No premedication required6
*A 3-5 minute injection time of OPDIVO Qvantig compared to 30-minute infusion time of OPDIVO. This does not account for all aspects of treatment and does not include observation time. Actual clinic time may vary.1,6

Safety Data
View a selected safety profile of adverse reactions seen in clinical trials.

Dosing Schedules
Find dosing information to get patients started on therapy.

More Gastroesophageal Indications
Learn more about other gastroesophageal indications across adjuvant and 1L metastatic settings.
Learn more about how OPDIVO is approved for use in earlier stages of cancer
References:
- OPDIVO [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.
- Kelly RJ, Ajani JA, Kuzdzal J, et al. Adjuvant nivolumab in resected esophageal or gastroesophageal junction cancer. N Engl J Med. 2021;384(13):1191-1203.
- Moehler M, Ajani JA, Kuzdzal J, et al. Adjuvant nivolumab in resected esophageal or gastroesophageal junction cancer following neoadjuvant chemoradiotherapy: 14-month follow-up of CheckMate 577. Presentation at ESMO 2021. Presentation 1381P.
- Data on file. NIVO 612. Princeton, NJ: Bristol-Myers Squibb Company; 2020.
- Data on file. BMS-REF-NIVO-0124. Princeton, NJ: Bristol-Myers Squibb Company; 2021.
- OPDIVO Qvantig [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.





