| BASELINE CHARACTERISTICS | OPDIVO (n=526) | PLACEBO (n=264) |
|---|---|---|
| Median age, years (range) | 62 (21-87) | 61 (19-92) |
| Male, n (%) | 322 (61%) | 161 (61%) |
| ECOG PS 0, n (%) | 495 (94%) | 245 (93%) |
Stage, n (%) IIB |
316 (60%) |
163 (62%) |
T category, n (%) T3b |
204 (39%) |
104 (39%) |
Melanoma subtype, n (%) Nodular |
266 (51%) |
133 (50%) |
Region, n (%) Western Europe |
303 (58%) |
160 (61%) |
OPDIVO Qvantig™ (nivolumab + hyaluronidase-nvhy) is approved as a subcutaneous injection
Approved in Stage IIB/C, III, IV
Adjuvant Treatment of Melanoma
Bring the benefit of OPDIVO® to more patients1

INDICATION OPDIVO® (nivolumab) is indicated for the adjuvant treatment of adult and pediatric patients 12 years and older with completely resected Stage IIB, Stage IIC, Stage III, or Stage IV melanoma.
Nivolumab (OPDIVO) is a NCCN Category 1 recommended adjuvant treatment option for completely resected pathological stage IIB/C cutaneous melanoma in the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®)2
NCCN=National Comprehensive Cancer Network® (NCCN®).
CHECKMATE 76K: IN ADULT AND PEDIATRIC PATIENTS 12 YEARS AND OLDER WITH COMPLETELY RESECTED STAGE IIB/C MELANOMA
Checkmate 76K evaluated RFS with OPDIVO q4w as adjuvant treatment for eligible patients with completely resected stage IIB/C melanoma1,3
PHASE 3, DOUBLE-BLIND, PLACEBO-CONTROLLED TRIAL1,3
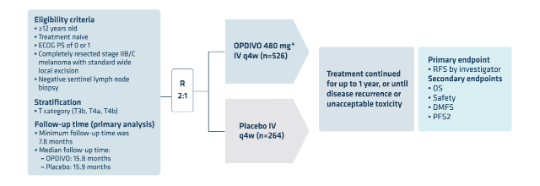
*See Full Prescribing Information for recommended dosing information.
DMFS=distant metastasis-free survival; ECOG PS=Eastern Cooperative Oncology Group Performance Score; IV=intravenous; OS=overall survival; PFS2=progression-free survival through next-line therapy; q4w=every 4 weeks; R=randomization; RFS=recurrence-free survival.
Patient baseline characteristics3
*Categorized as desmoplastic melanoma (n=21 [4%]), lentigo maligna (n=13 [2%]), “other” (n=44 [8%]), and not reported (n=3 [1%]).
†Categorized as desmoplastic melanoma (n=8 [3%]), lentigo maligna (n=3 [1%]), “other” (n=22 [8%]), and not reported (n=1 [<1%]).
Select Important Safety Information
Serious Adverse Reactions
In Checkmate 76K, serious adverse reactions occurred in 18% of patients receiving OPDIVO (n=524). Adverse reactions which resulted in permanent discontinuation of OPDIVO in >1% of patients included arthralgia (1.7%), rash (1.7%), and diarrhea (1.1%). A fatal adverse reaction occurred in 1 (0.2%) patient (heart failure and acute kidney injury). The most frequent Grade 3-4 lab abnormalities reported in ≥1% of OPDIVO-treated patients were increased lipase (2.9%), increased AST (2.2%), increased ALT (2.1%), lymphopenia (1.1%), and decreased potassium (1.0%).
Please see additional Important Safety Information below.
At the primary analysis, OPDIVO reduced the risk of recurrence* or death by 58% compared to placebo1,3
AT THE ~34-MONTH MEDIAN FOLLOW-UP, THE RFS HR WAS 0.62 FOR OPDIVO VS PLACEBO4†
RECURRENCE-FREE SURVIVAL RESULTS AT ~34-MONTH MEDIAN FOLLOW-UP ANALYSIS1,3,4†‡
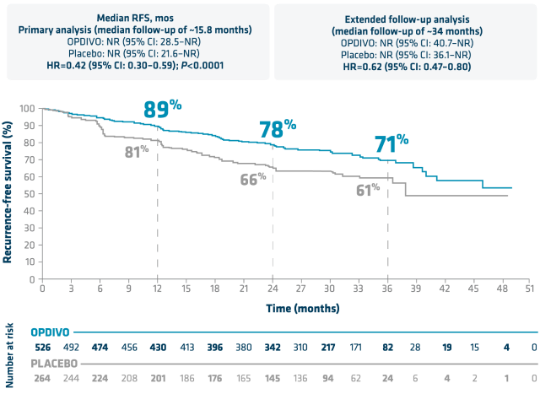
*Recurrence includes new primary melanoma.1
†Median follow-up was 34.2 months for the OPDIVO group and 33.9 months for the placebo group.4
‡The follow-up analysis is not powered to assess statistical significance.
RFS is defined as the time between the date of randomization and the date of first recurrence (local, regional, or distant metastasis), new primary melanoma, or death, from any cause, whichever occurred first and as assessed by the investigator.1
CI=confidence interval; HR=hazard ratio; NR=not reached.
At ~34-month median follow-up, an HR of 0.72 was observed for DMFS for OPDIVO vs placebo4*
SECONDARY ENDPOINT: DMFS RESULTS AT ~34-MONTH MEDIAN FOLLOW-UP ANALYSIS4*
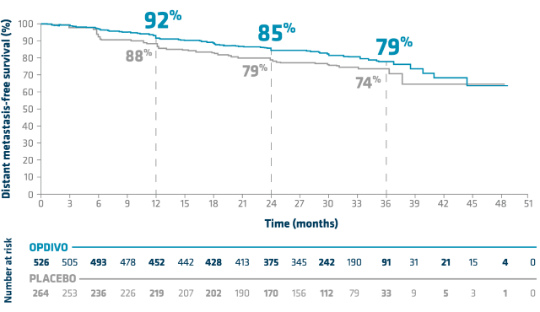
- HR vs placebo (95% CI): 0.72 (0.52–1.00)4
- Median DMFS, mos (95% CI): NR with OPDIVO (n=526) and NR with placebo (n=264)4
- DMFS was not assessed for statistical significance4
DMFS is defined as the time between the date of randomization and the date of first distant metastasis or date of death (whichever the cause), whichever occurred first.5
*Median follow-up was 34.2 months for the OPDIVO group and 33.9 months for the placebo group.4
NA=not available.
Select Important Safety Information
Common Adverse Reactions
In Checkmate 76K, the most common adverse reactions (≥20%) reported with OPDIVO (n=524) were fatigue (36%), musculoskeletal pain (30%), rash (28%), diarrhea (23%) and pruritis (20%).
Please see additional Important Safety Information below.
Higher RFS rates observed regardless of disease stage or T category with OPDIVO4*†
RFS DATA BY SUBGROUP WITH UNSTRATIFIED HR AT ~34-MONTH MEDIAN FOLLOW-UP ANALYSIS4†
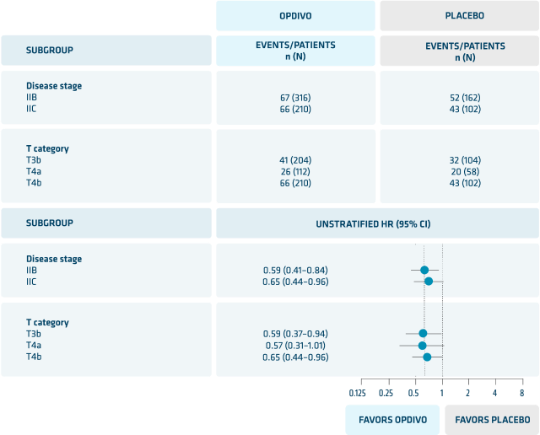
These analyses were exploratory and not powered.
*vs placebo.
†Median follow-up was 34.2 months for the OPDIVO group and 33.9 months for the placebo group.4
N=number.
OPDIVO Qvantig monotherapy dosing6
OPDIVO is still available as an IV infusion. View OPDIVO IV dosing schedule >
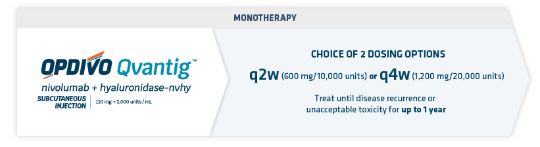
INDICATION OPDIVO Qvantig (nivolumab + hyaluronidase-nvhy), as monotherapy, is indicated for the adjuvant treatment of adult patients with completely resected Stage IIB, Stage IIC, Stage III, or Stage IV melanoma.
- OPDIVO Qvantig is administered as a 3- to 5-minute subcutaneous injection6
- Review the Full US Prescribing Information for recommended dosage information for OPDIVO Qvantig
- No premedication required6
CHECKMATE 238: ADJUVANT TREATMENT OF MELANOMA
The only head-to-head clinical trial to evaluate a current standard of care vs an active comparator with proven OS benefit*1,2,7-9,11
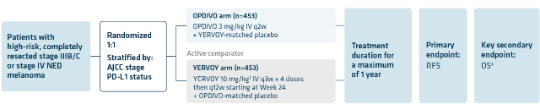
Similar to the real-world population, Checkmate 238 included 42% BRAF mutant patients1,10
*Study CA 184-029 originally compared YERVOY® (ipilimumab) 10mg/kg vs. placebo.8 Based on the efficacy analysis for Study E1609, the OS HR of YERVOY 3mg/kg vs high-dose interferon (HDI) was 0.78 (95% CI, 0.61-0.99); P=0.044. The 5-year OS rate was 72% (95% CI, 68-76) in the ipilimumab group, as compared with 67% (95% CI, 62-71) in the HDI group.11
†YERVOY 10mg/kg is currently not an approved adjuvant melanoma dose.8,11
‡OS in Checkmate 238 did not meet statistical significance.1
AJCC=American Joint Committee on Cancer; BRAF=B-Raf proto-oncogene; CI=confidence interval; HR=hazard ratio; IV=intravenous; NED=no evidence of disease; OS=overall survival; PD-L1=programmed death-ligand 1; q2w=every 2 weeks; q3w=every 3 weeks; q12w=every 12 weeks; RFS=recurrence-free survival.
Select Important Safety Information
Serious Adverse Reactions
In Checkmate 238, serious adverse reactions occurred in 18% of patients receiving OPDIVO® (n=452). Grade 3 or 4 adverse reactions occurred in 25% of OPDIVO-treated patients (n=452). The most frequent Grade 3 and 4 adverse reactions reported in ≥2% of OPDIVO-treated patients were diarrhea and increased lipase and amylase.
Please see additional Important Safety Information below.
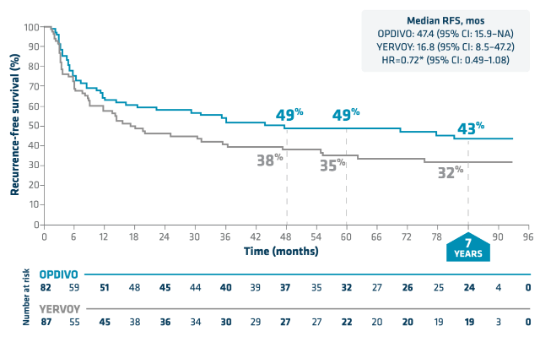
Durable RFS benefit and the longest follow-up for any PD-1 agent in the adjuvant setting for melanoma1,7,9,12-14
RECURRENCE-FREE SURVIVAL RESULTS THROUGH 7 YEARS
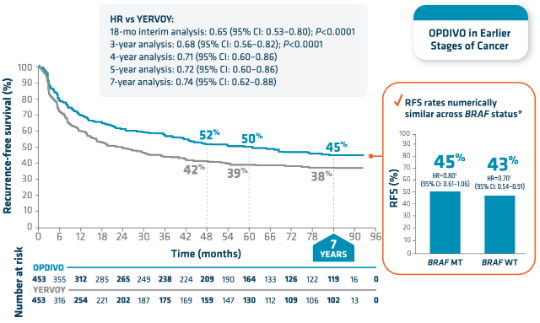
Median RFS, mos (95% CI):
- 18 months (ITT): OPDIVO 3 mg/kg: NR (NR–NR); YERVOY 10 mg/kg: NR (16.6–NR)1,9
- 7 years (ITT): OPDIVO 3 mg/kg: 61.1 (42.9–NR); YERVOY 10 mg/kg: 24.2 (16.6–35.1)7
- RFS by BRAF status was an exploratory pre-specified subgroup analysis at 18 months and at 7 years1,7,9
- 7-year RFS rate in patients receiving YERVOY was 39%* for BRAF MT and 35%* for BRAF WT7
- 7-year RFS in BRAF MT: 68.6 for OPDIVO (35.0–NR), 25.5 for YERVOY (15.9–55.1)7
- 7-year RFS in BRAF WT: 50.2 for OPDIVO (36.3–NR), 16.6 for YERVOY (11.6–35.1)7
*These data are based on RFS Kaplan-Meier estimates.7
†Unstratified hazard ratio.7
ITT=intent to treat; MT=mutant; NR=not reached; PD-1=programmed cell death protein-1; WT=wild-type.
Select Important Safety Information
Common Adverse Reactions
In Checkmate 238, the most common adverse reactions (≥20%) reported in OPDIVO-treated patients (n=452) vs ipilimumab-treated patients (n=453) were fatigue (57% vs 55%), diarrhea (37% vs 55%), rash (35% vs 47%), musculoskeletal pain (32% vs 27%), pruritus (28% vs 37%), headache (23% vs 31%), nausea (23% vs 28%), upper respiratory infection (22% vs 15%), and abdominal pain (21% vs 23%). The most common immune-mediated adverse reactions were rash (16%), diarrhea/colitis (6%), and hepatitis (3%).
Please see additional Important Safety Information below.
RFS rates were numerically similar across BRAF status through 7 years7
RFS IN BRAF MUTANT

RFS IN BRAF WILD-TYPE

RFS by BRAF status was an exploratory pre-specified analysis at 18 months and 7 years.7,9
*Unstratified hazard ratio.7
N=number.
Recurrence-free survival in patients with stages III and IV (NED) through 7 years15
Stage IIIB/C RFS
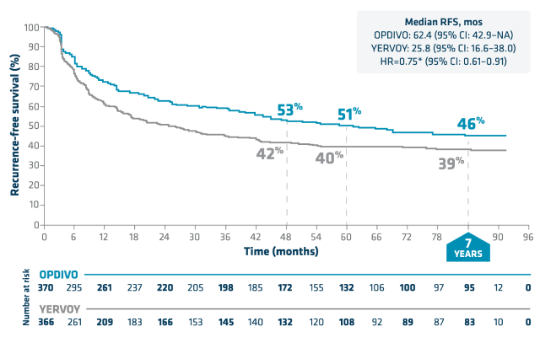
Stage IV (NED) RFS
STAGE IIIB/C RFS AT 7-YEAR FOLLOW-UP ANALYSIS
- Stage IIIB: 53%† for OPDIVO vs 46%† for YERVOY; HR=0.73 (95% CI: 0.53–1.01)7
- Stage IIIC: 39%† for OPDIVO vs 34%† for YERVOY; HR=0.78 (95% CI: 0.60–1.00)7
- Not reported: 1 of 1 for OPDIVO and 0 of 0 for YERVOY7
- RFS by stages IIIB/C and IV (NED) was a post hoc analysis at 7 years. Melanoma stages IIIB, IIIC, and IV (NED) were assessed per AJCC 7th edition1,7
*Unstratified HR.15
†These data are based on RFS Kaplan-Meier estimates.15
NA=not available.
OPDIVO Qvantig monotherapy dosing6
OPDIVO is still available as an IV infusion. View OPDIVO IV dosing schedule >
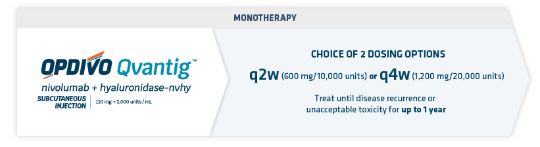
INDICATION OPDIVO Qvantig (nivolumab + hyaluronidase-nvhy), as monotherapy, is indicated for the adjuvant treatment of adult patients with completely resected Stage IIB, Stage IIC, Stage III, or Stage IV melanoma.
- OPDIVO Qvantig is administered as a 3- to 5-minute subcutaneous injection6
- Review the Full US Prescribing Information for recommended dosage information for OPDIVO Qvantig
- No premedication required6
q4w dosing offers a balance for both patient and provider needs1,16

Balance extended time between infusions with the confidence of regular monitoring
Help control patient adherence concerns with IV administration regardless of BRAF mutation status1
- Infusions may reduce adherence concerns and can be coordinated with patients’ monthly follow-up visits16
- No in-home refrigeration, meal restrictions, and/or treatment pill burden for patients1*‡
*This content is not intended to imply comparative efficacy between OPDIVO dosing schedules. Selection of approved dosing frequency should be based on independent clinical judgment.
†For pediatric patients age 12 years and older and weighing less than 40 kg, OPDIVO dosing is 3 mg/kg every 2 weeks or 6 mg/kg every 4 weeks (30-minute IV infusion) until disease recurrence or unacceptable toxicity for up to 1 year.1
‡Please see the OPDIVO Full Prescribing Information for guidance on storage and refrigeration.

Safety Data
View a selected safety profile of adverse reactions seen in clinical trials.

Dosing Schedules
Find dosing information to get patients started on therapy.

More Melanoma Options
Learn more about all melanoma indications.
Learn more about how OPDIVO is approved for use in earlier stages of cancer
References:
- OPDIVO [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Melanoma: Cutaneous V.3.2024. ©National Comprehensive Cancer Network, Inc. 2024. All rights reserved. Accessed September 24, 2024. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Kirkwood JM, Del Vecchio M, Weber J, et al. Adjuvant nivolumab in resected stage IIB/C melanoma: primary results from the randomized, phase 3 CheckMate 76K trial. Nat Med. 2023;29(11):2835-2843.
- Long GV, Del Vecchio M, Hoeller C, et al. Adjuvant nivolumab versus placebo in stage IIB/C melanoma: 3-year results from CheckMate 76K. Presented at ESMO 2024. Presentation number 1077MO.
- Effectiveness study of nivolumab compared to placebo in prevention of recurrent melanoma after complete resection of stage IIB/C melanoma (CheckMate76K). ClinicalTrials.gov identifier: NCT04099251. https://classic.clinicaltrials.gov/ct2/show/NCT04099251. Updated July 27, 2023. Accessed August 10, 2023.
- OPDIVO Qvantig [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.
- Ascierto PA, Del Vecchio M, Merelli B, et al. Adjuvant nivolumab versus ipilimumab in resected stage III/IV melanoma: 7-year results from CheckMate 238. Presented at ESMO 2023. Abstract 1089P.
- Eggermont AMM, Chiarion-Sileni V, Grob J-J, et al. Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N Engl J Med. 2016;375(19):1845-1855.
- Weber J, Mandala M, Del Vecchio M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377(19):1824-1835.
- Cheng L, Lopez-Beltran A, Massari F, MacLennan GT, Montironi R. Molecular testing for BRAF mutations to inform melanoma treatment decisions: a move toward precision medicine. Mod Pathol. 2018;31(1):24-38.
- YERVOY [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2023.
- Ascierto PA, Del Vecchio M, Mandalá M, et al. Adjuvant nivolumab versus ipilimumab in resected stage IIIB-C and stage IV melanoma (CheckMate 238): 4-year results from a multicentre, double-blind, randomised, controlled, phase 3 trial. Lancet Oncol. 2020;21(11):1465-1477.
- Weber J, Del Vecchio M, Mandala M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III/IV melanoma: 3-year efficacy and biomarker results from the phase 3 CheckMate 238 trial. Presented at ESMO 2019. Abstract 2801.
- Weber J, Larkin J, Mandalá M, et al. Five-year outcomes with adjuvant nivolumab versus ipilimumab in resected stage IIIB-C or IV melanoma (CheckMate 238). Oral presentation at SMR 2021.
- Data on file. BMS-REF-NIVO-0253. Princeton, NJ: Bristol-Myers Squibb Company; 2023.
- Seal BS, Anderson S, Shermock KM. Factors associated with adherence rates for oral and intravenous anticancer therapy in commercially insured patients with metastatic colon cancer. J Manag Care Spec Pharm. 2016;22(3):227-235.
Indications
YERVOY® (ipilimumab), as a single agent or in combination with nivolumab, is indicated for the treatment of unresectable or metastatic melanoma in adult and pediatric patients 12 years and older.
YERVOY® (ipilimumab) is indicated for the adjuvant treatment of adult patients with cutaneous melanoma with pathologic involvement of regional lymph nodes of more than 1 mm who have undergone complete resection, including total lymphadenectomy.
YERVOY Important Safety Information
Severe and Fatal Immune-Mediated Adverse Reactions
Immune-mediated adverse reactions listed herein may not be inclusive of all possible severe and fatal immune- mediated adverse reactions.
Immune-mediated adverse reactions, which may be severe or fatal, can occur in any organ system or tissue. While immune-mediated adverse reactions usually manifest during treatment, they can also occur at any time after starting or discontinuing YERVOY. Early identification and management are essential to ensure safe use of YERVOY. Monitor for signs and symptoms that may be clinical manifestations of underlying immune-mediated adverse reactions. Evaluate clinical chemistries including liver enzymes, creatinine, adrenocorticotropic hormone (ACTH) level, and thyroid function at baseline and before each dose. Institute medical management promptly, including specialty consultation as appropriate.
Withhold or permanently discontinue YERVOY depending on severity (please see section 2 Dosage and Administration in the accompanying Full Prescribing Information). In general, if YERVOY interruption or discontinuation is required, administer systemic corticosteroid therapy (1 or 2 mg/kg/day prednisone or equivalent) until improvement to Grade 1 or less. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Consider administration of other systemic immunosuppressants in patients whose immune-mediated adverse reactions are not controlled with corticosteroid therapy. Toxicity management guidelines for adverse events that do not necessarily require systemic corticosteroids (e.g., endocrinopathies) are discussed below.
Immune-Mediated Colitis
YERVOY can cause immune-mediated colitis, which may be fatal. Cytomegalovirus (CMV) infection/reactivation has been reported in patients with corticosteroid-refractory immune-mediated colitis. In cases of corticosteroid-refractory colitis, consider repeating infectious workup to exclude alternative etiologies. Immune-mediated diarrhea/colitis occurred in 12% (62/511) of patients who received YERVOY 3 mg/kg as a single agent, including Grade 3-5 (7%) and Grade 2 (5%).
Immune-Mediated Hepatitis
Immune-mediated hepatitis occurred in 4.1% (21/511) of patients who received YERVOY 3 mg/kg as a single agent, including Grade 3-5 (1.6%) and Grade 2 (2.5%).
Immune-Mediated Dermatologic Adverse Reactions
YERVOY can cause immune-mediated rash or dermatitis, including bullous and exfoliative dermatitis, Stevens Johnson Syndrome, toxic epidermal necrolysis (TEN), and DRESS (drug rash with eosinophilia and systemic symptoms). Topical emollients and/or topical corticosteroids may be adequate to treat mild to moderate non- bullous/exfoliative rashes. Immune-mediated rash occurred in 15% (76/511) of patients who received YERVOY 3 mg/kg as a single agent, including Grade 3-5 (2.5%) and Grade 2 (12%).
Immune-Mediated Endocrinopathies
Grade 2-5 immune-mediated endocrinopathies occurred in 4% (21/511) of patients who received YERVOY 3 mg/kg as a single agent. Severe to life-threatening (Grade 3-4) endocrinopathies occurred in 9 patients (1.8%). All 9 of these patients had hypopituitarism with some patients having additional concomitant endocrinopathies, such as adrenal insufficiency, hypogonadism, and hypothyroidism. Six of the 9 patients were hospitalized for severe endocrinopathies. Moderate (Grade 2) endocrinopathy occurred in 12 patients (2.3%), including hypothyroidism, adrenal insufficiency, hypopituitarism, hyperthyroidism and Cushing’s syndrome. YERVOY can cause immune-mediated hypophysitis. Hypophysitis can present with acute symptoms associated with mass effect such as headache, photophobia, or visual field cuts. Hypophysitis can cause hypopituitarism. Initiate hormone replacement as clinically indicated.
Other Immune-Mediated Adverse Reactions
Across clinical trials of YERVOY administered as a single agent or in combination with nivolumab, the following clinically significant immune-mediated adverse reactions, some with fatal outcome, occurred in <1% of patients unless otherwise specified, as shown below:
Nervous System: Autoimmune neuropathy (2%), meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis, Guillain-Barré syndrome, nerve paresis, motor dysfunction
Cardiovascular: Angiopathy, myocarditis, pericarditis, temporal arteritis, vasculitis
Ocular: Blepharitis, episcleritis, iritis, orbital myositis, scleritis, uveitis. Some cases can be associated with retinal detachment. If uveitis occurs in combination with other immune-mediated adverse reactions, consider a Vogt- Koyanagi-Harada–like syndrome, which has been observed in patients receiving YERVOY and may require treatment with systemic corticosteroids to reduce the risk of permanent vision loss.
Gastrointestinal: Duodenitis, gastritis, pancreatitis (1.3%)
Musculoskeletal and Connective Tissue: Arthritis, myositis, polymyalgia rheumatica, polymyositis, rhabdomyolysis
Other (hematologic/immune): Aplastic anemia, conjunctivitis, cytopenias (2.5%), eosinophilia (2.1%), erythema multiforme, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), hypersensitivity vasculitis, meningitis, neurosensory hypoacusis, psoriasis, sarcoidosis, systemic inflammatory response syndrome, and solid organ transplant rejection.
Infusion-Related Reactions
Severe infusion-related reactions can occur with YERVOY. Discontinue YERVOY in patients with severe or life- threatening (Grade 3 or 4) infusion reactions. Interrupt or slow the rate of infusion in patients with mild or moderate (Grade 1 or 2) infusion reactions. Infusion-related reactions occurred in 0.6% (3/511) of patients who received single-agent YERVOY 3 mg/kg for the unresectable or metastatic treatment of melanoma.
Complications of Allogeneic Hematopoietic Stem Cell Transplant after YERVOY
Fatal or serious graft-versus-host disease (GVHD) can occur in patients who receive YERVOY either before or after allogeneic hematopoietic stem cell transplantation (HSCT). These complications may occur despite intervening therapy between CTLA-4 receptor blocking antibody and allogeneic HSCT. Follow patients closely for evidence of GVHD and intervene promptly. Consider the benefit versus risks of treatment with YERVOY after allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action, YERVOY can cause fetal harm when administered to a pregnant woman. The effects of YERVOY are likely to be greater during the second and third trimesters of pregnancy. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with YERVOY and for 3 months after the last dose.
Lactation
There are no data on the presence of YERVOY in human milk or its effects on the breastfed child or milk production. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed during treatment with YERVOY and for 3 months following the last dose.
Common Adverse Reactions
The most common adverse reactions (≥20%) with YERVOY as a single agent are fatigue, diarrhea, pruritis, rash, nausea, and headache.
Please see US Full Prescribing Information.





