| Baseline characteristics | OPDIVO + Chemotherapy† (n=304) |
Chemotherapy† (n=304) |
|---|---|---|
| Median age (range), years | 65 (32-86) | 65 (35-85) |
| Male, % | 77.6 | 77.0 |
Region, % United States |
6.2 44.1 23.7 26.0 |
6.9 46.7 20.1 26.3 |
| ECOG PS, % 0 1 >1 |
53.3 46.1 0.7 |
53.3 46.7 0.0 |
| Tumor type at initial diagnosis, (%) Urinary bladder Renal pelvis Other |
77.3 10.9 11.8 |
72.0 14.5 13.5 |
| Disease stage, % Metastatic Locally unresectable or nonmetastatic Not reported |
85.9 13.5 0.7 |
88.5 10.9 0.7 |
| Tumor PD-L1 expression, % ≥1% <1% |
36.5 63.5 |
36.2 63.8 |
| Liver metastases, % Yes No |
21.1 78.9 |
21.1 78.9 |
OPDIVO Qvantig™ (nivolumab + hyaluronidase-nvhy) is approved as a subcutaneous injection
1L Treatment of Unresectable or Metastatic UC
A chance to deliver a proven combination—right from the start 1,2
In the 1L treatment of adult patients with unresectable or metastatic urothelial carcinoma, OPDIVO® + chemotherapy* is the first and only FDA-approved upfront I-O + chemotherapy combination

*Cisplatin and gemcitabine.1
1L=first-line; I-O=immuno-oncology.
INDICATION OPDIVO® (nivolumab), in combination with cisplatin and gemcitabine, is indicated for the first-line treatment of adult patients with unresectable or metastatic urothelial carcinoma.
Unmet need still remains in the treatment of 1L mUC2,3

mUC=metastatic urothelial carcinoma.
Scroll down to learn more about Checkmate 901
CHECKMATE 901: 1L TREATMENT OF ADULT PATIENTS WITH UNRESECTABLE OR METASTATIC UROTHELIAL CARCINOMA
A phase 3 global study in 1L unresectable or mUC comparing upfront OPDIVO + chemotherapy followed by OPDIVO monotherapy vs chemotherapy alone1,2*
CHECKMATE 901 STUDY DESIGN1,2
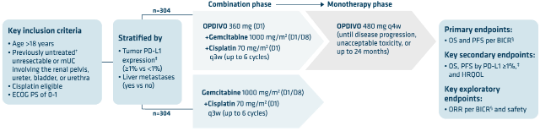
OPDIVO + chemotherapy has a finite duration of treatment, with up to 6 cycles of OPDIVO + chemotherapy followed by OPDIVO monotherapy for up to 2 years1*
- Patients discontinuing cisplatin alone were permitted to switch to carboplatin2
- Patients with active CNS metastases were excluded1
- Median follow-up time of the primary analysis was 33.6 months (range: 7.4–62.4)2
*Cisplatin and gemcitabine.1
†Prior neoadjuvant or adjuvant chemotherapy were permitted as long as the disease recurrence took place ≥12 months from completion of therapy.1
‡PD-L1 status was defined by the percentage of positive tumor cell membrane staining in a minimum of 100 tumor cells that could be evaluated with the use of the Dako PD-L1 IHC 28-8 pharmDx immunohistochemical assay.2
§According to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1.1
BICR=blinded independent central review; CNS=central nervous system; D=day; ECOG PS=Eastern Cooperative Oncology Group Performance Status; HRQOL=health-related quality of life; IHC=immunohistochemistry; ORR=overall response rate; OS=overall survival; PD-L1=programmed death-ligand 1; PFS=progression-free survival; q3w=every three weeks; q4w=every four weeks.
Select Important Safety Information
Serious Adverse Reactions
In Checkmate 901, serious adverse reactions occurred in 48% of patients receiving OPDIVO in combination with chemotherapy. The most frequent serious adverse reactions reported in ≥2% of patients who received OPDIVO with chemotherapy were urinary tract infection (4.9%), acute kidney injury (4.3%), anemia (3%), pulmonary embolism (2.6%), sepsis (2.3%), platelet count decreased (2.3%). Fatal adverse reactions occurred in 3.6% of patients who received OPDIVO in combination with chemotherapy; these included sepsis (1%). OPDIVO and/or chemotherapy were discontinued in 30% of patients and were delayed in 67% of patients for an adverse reaction.
Common Adverse Reactions
In Checkmate 901, the most common adverse reactions (≥20%) were nausea, fatigue, musculoskeletal pain, constipation, decreased appetite, rash, vomiting, and peripheral neuropathy.
Please see additional Important Safety Information below and U.S. Full Prescribing Information for OPDIVO.
Baseline characteristics2*
*At least one dose of carboplatin was received instead of cisplatin in 49 of 304 treated patients (16.1%) in the nivolumab-combination group and in 43 of 288 treated patients (14.9%) in the gemcitabine-cisplatin group.2
†Cisplatin and gemcitabine.1
In the 1L treatment of adult patients with unresectable or metastatic UC
The only I-O + chemotherapy combination that demonstrated significantly longer overall survival vs chemotherapy alone1,2*†
MEDIAN OVERALL SURVIVAL IN THE ITT POPULATION (MEDIAN FOLLOW-UP TIME OF 33.6 MONTHS)1,2

*Cisplatin and gemcitabine.1
†In a phase 3 trial.2
CI=confidence interval; HR=hazard ratio; I-O=immuno-oncology; ITT=intention to treat.
OPDIVO + chemotherapy reduced the risk of disease progression or death by 28% vs chemotherapy alone1,2*
PROGRESSION-FREE SURVIVAL IN THE ITT POPULATION (MEDIAN FOLLOW-UP TIME OF 33.6 MONTHS)1,2†

*Cisplatin and gemcitabine.1
†Assessed by BICR.1
Deep and durable complete responses observed with patients on OPDIVO + chemotherapy1,2*
Exploratory endpoint: ORR† at primary analysis (median follow-up time of 33.6 months): 57.6% (n=175; 95% CI: 51.8–63.2) for OPDIVO + chemotherapy and 43.1% (n=131; 95% CI: 37.5–48.9) for chemotherapy; 22% CR (n=66) and 36% PR (n=109) for OPDIVO + chemotherapy and 12% CR (n=36) and 31% PR (n=95) for chemotherapy1,2‡

Median DOR at primary analysis (median follow-up time of 33.6 months)2
- OPDIVO + chemotherapy: 9.5 months (95% CI: 7.6–15.1)
- Chemotherapy: 7.3 months (95% CI: 5.7–8.9)
*Cisplatin and gemcitabine.1
†Assessed by BICR.1
‡ORR was an exploratory endpoint. The study was not powered to detect a difference between treatment arms in relation to CR or duration of CR and results should be interpreted with caution.
CR=complete response; DOR=duration of response; NE=not estimable; PR=partial response.
With OPDIVO + chemotherapy, there was a 35% chance for responses to last 2 years1,4*
Exploratory endpoint: ORR† at primary analysis (median follow-up time of 33.6 months): 57.6% (n=175; 95% CI: 51.8–63.2) for OPDIVO + chemotherapy and 43.1 (n=131; 95% CI: 37.5–48.9) for chemotherapy; 22% CR (n=66) and 36% PR (n=109) for OPDIVO + chemotherapy and 12% CR (n=36) and 31% PR (n=95) for chemotherapy1,2‡
DURATION OF RESPONSE IN THE ITT POPULATION (MEDIAN FOLLOW-UP TIME OF 33.6 MONTHS)1,4

ORR was an exploratory endpoint. The study was not powered to detect a difference between treatment arms in relation to ORR or DOR and results should be interpreted with caution.
*Cisplatin and gemcitabine.1
†Assessed by BICR.1
‡ORR was an exploratory endpoint. The study was not powered to detect a difference between treatment arms in relation to CR or duration of CR and results should be interpreted with caution.
OPDIVO Qvantig + chemotherapy* followed by OPDIVO Qvantig monotherapy provides multiple dosing options5
OPDIVO is still available as an IV infusion. View OPDIVO IV dosing schedule >
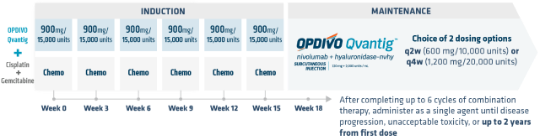
INDICATION OPDIVO Qvantig (nivolumab + hyaluronidase-nvhy), in combination with cisplatin and gemcitabine, is indicated for the first-line treatment of adult patients with unresectable or metastatic UC.
- OPDIVO Qvantig is administered as a 3- to 5-minute subcutaneous injection5
- The first dose of OPDIVO Qvantig monotherapy should be administered after completing 6 doses of the OPDIVO Qvantig and cisplatin + gemcitabine chemotherapy combination5
- Review the US Full Prescribing Information for OPDIVO Qvantig for recommended dosage information
- No premedication required5
*Cisplatin and gemcitabine.1,5

Safety Data
View a selected safety profile of adverse reactions seen in clinical trials.

Dosing Schedules
Find dosing information to get patients started on therapy.

More UC Indications
Learn about another urothelial carcinoma indication.
References:
- OPDIVO [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.
- van der Heijden MS, Sonpavde G, Powles T, et al. Nivolumab plus gemcitabine–cisplatin in advanced urothelial carcinoma. N Engl J Med. 2023;389(19):1778-1789.
- Alimohamed N, Grewal S, Wirtz HS, et al. Understanding treatment patterns and outcomes among patients with de novo unresectable locally advanced or metastatic urothelial cancer: a population-level retrospective analysis from Alberta, Canada. Curr Oncol. 2022;29(10):7587-7597.
- van der Heijden MS, Sonpavde G, Powles T, et al. Nivolumab plus gemcitabine-cisplatin in advanced urothelial carcinoma [suppl]. N Engl J Med. 2023;389(19):1778-1789.
- OPDIVO Qvantig [package insert]. Princeton, NJ: Bristol-Myers Squibb Company.





